Arthrosis
Arthrosis is one of several types of arthritis – a disease that causes joint inflammation. Also known as osteoarthritis, it is a degenerative and progressive pathology caused by increased bone friction. Increased joint friction can lead to local inflammation, causing pain, swelling, and functional limitations. In addition, according to the study “Thermotherapy for treatment of osteoarthritis”, it can evolve quickly and destroy the entire cartilage.
American studies indicate that more than 50 million people have this disease. It is one of the most frequent causes of pain in the musculoskeletal system and the incapacity to work worldwide. Osteoarthritis is also the most prevalent rheumatic disease in the population over 65. Years ago, this pathology was considered a slowly progressive disease with no treatment prospect, usually seen as a consequence of the natural aging process. However, nowadays, it is possible to modify the course of the disease in terms of immediate symptomatic treatment and prognosis. To better understand the deterioration process that occurs in osteoarthritis, it is necessary to know how a joint works:
An articulation, or joint (as it is popularly known), is where the bones meet. Some joints examples are the knee, which connects the femur and tibia bones, putting the thigh and the leg together; the ankle, which articulates the tibia, fibula, and talus bones, joining the legs to the feet; the elbow, which links the humerus bone to the ulna and radius bones, colligating the upper arm to the forearm. These structures are covered by cartilage and soften friction by reducing the direct impact between bone ends, preventing joint damage. They allow the bones to slide over each other with little friction by dampening. Thus, when the joint loses this cartilage, arthrosis is established. Joint insufficiency, caused by the imbalance between the formation and reabsorption of its main elements, associated with various conditions, leads to joint pain.
The cartilage becomes rougher at the onset of osteoarthritis, leading to increased friction when moving the joint. Severe osteoarthritis occurs when the cartilage is destroyed, causing intense bone friction.
TYPES OF ARTHROSIS
Osteoarthritis can be classified into two types:
– Primary: when there is no specific cause for the onset of cartilage wear, and it is associated with excessive joint use, such as advanced age, overweight, and intensive practice of high-impact physical activities;
– Secondary: when some factor marked the beginning of cartilage wear, such as joint fractures, diseases, and deformities. The starting point of the disease is the increased load or failures on the joint’s protective factors (muscles, ligaments, joint capsule, menisci), leaving it vulnerable to cartilage wear.
CLASSIFICATION OF ARTHROSIS
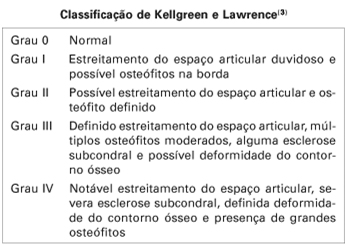
Identifying the degree of joint impairment is essential for treatment since this disease is progressive. It begins with a reduction in the joint’s space, which has lost stability and may present osteophytes (bone growth around the joint) in an attempt to restore the lost equilibrium. At the most severe level of the disease, the joint space is virtually gone, and the joint has large bone spurs and may crepitate, crack or creak. There is also movement loss and stiffness that worsens in the cold. Therefore, osteoarthritis is classified as follows:
CAUSES
Osteoarthritis is a multifactorial disease, so it depends on several factors combined. For example, it may be associated with age, genetics, gender, ethnicity, bone density, nutritional and metabolic factors, or external factors such as daily activities and biomechanical factors.
The main mechanical factors are:
– Joint misalignment: causes increased impact and degenerative process;
– Overload: can be derived from the overweight or increased physical activity without adequate preparation;
– Muscle weakness: muscle is the primary protection of joints. The weaker it is, the greater the chance of arthrosis developing;
– Alteration in the foot type (flat or cavus): causes misalignment and joint wear. The older a person is, the more likely they are to develop flat feet and harmful misalignment;
– Previous surgeries: some surgical processes, such as the menisci removal or ligament reconstruction, can make the joint unstable and lead to arthrosis;
– Trauma and joint injuries: previous injuries can make the joint unstable and vulnerable to disease.
The following are considered vulnerability factors:
– Age: advanced age increases predisposition to the disease since the wear is characteristic;
– Heredity and sex: women whose mothers have arthrosis are more likely to develop the pathology;
– Obesity: obese people have increased joint load, leading to degenerative phenomena;
– Hypermobility: it implies extra joint stress and ease in cartilage rupture;
- Limb discrepancy or dysplasia: causes misalignment of the joint surface, leading to early arthrosis;
– Hormonal Factors: hormonal imbalances alter bone metabolism, leading to the development of the disease.
SIGNS AND SYMPTOMS
Osteoarthritis can evolve without symptoms and be diagnosed only in more advanced stages. Still, there are some signs to identify it, such as crackling or creaking in the joint during movement.
The pain is often worse at the end of the day and after long inactive periods with mobility reduction, swelling, local heat, and crackles during movement. Some people also feel more pain with climate change. As osteoarthritis progresses, pain arises with increasingly less intense activities and can occur even at rest and during the night. Osteoarthritis in advanced stages leads to severe disabilities.
The pain is not caused by damage to the cartilage, as it has no innervation. It means some people with severe cartilage damage may have few pain complaints. People with less visible cartilage damage may have more pronounced symptoms due to joint instability and inflammation of the surrounding tissues. The main symptom of osteoarthritis is pain, and it may be related to the following:
– Rigidity of the joint’s surrounding musculature;
– Decreased muscle strength;
– Loss of movement range;
– Balance loss in case the joint helps support the body weight, such as the ankle, knee, and hip;
Joint stiffness is also a very usual complaint in people with osteoarthritis. Stiffness is expected in the first minutes of the day, after waking up, improving with time. However, episodes of joint stiffness may also appear during the day, especially after long periods of inactivity.
PREVENTION AND TREATMENT
Only a specialist can diagnose arthrosis by assessing the affected region’s sensitivity and the joint’s range of movement. The patient and family history will also be analyzed (to check the hereditary factor), along with pain occurrence and duration. Imaging exams can indicate wear in the areas where the patient feels discomfort and illustrate the disease development stage. The x-ray, even if it does not show the cartilage, can be very useful for diagnosing arthrosis in advanced cases.
Arthrosis is a chronic disease that progressively worsens over the years. Treatment slows the progression of the pathology and helps reduce symptoms. It includes therapies, medications, and surgery in some cases. Conservative treatment aims to control pain and swelling, improve quality of life, and prevent disease progression. In general, the prevention and treatment of arthrosis are related to joint mobility gain, stability, and improved alignment, so it is necessary to increase balance and muscle strength. We can take some measures to control the disease, such as:
– Physiotherapy: will indicate specific exercises to strengthen the muscles close to the affected area and reduce pain by using specific devices (TENS, US, laser) and improving the patient’s posture for daily activities (correct way of walking, sweeping the house without overloading the spine or knees, the way to sit, etc.);
– Weight loss: decreases joint overload (mainly applicable to overweight people). Weight excess is associated with a higher probability of developing arthrosis, especially in the knees;
– Rest: osteoarthritis pain usually worsens after exertion and improves after rest. Resting the joint affected in times of crisis helps relieve pain. However, excessive rest can atrophy the muscles and reduce joint mobility. Therefore, short periods of absolute rest are recommended, generally in acute cases of pain;
– Decrease the practice of high-impact physical activity: some physical activities require repeated and high-impact movements, which can accelerate cartilage wear, can lead to joint wear. Joints lose cartilage more quickly, which decreases their ability to absorb impact;
– Practicing physical activity: physical exercises are essential for people with arthrosis. Despite the discomfort that moving the affected joints causes during exertion, physical activity strengthens the muscles around your joint and increases the range of motion. The more robust and flexible the musculature, the less friction between the bones and, consequently, the less pain and inflammation;
– Ice packs are widely used for pain relief and inflammatory control. Some studies have shown improvement in joint mobility with the application of compresses combined with kinesiotherapy (exercise therapy);
– Medicines: should only be used with medical indication. The most common are analgesics to reduce pain and anti-inflammatories to control inflammatory processes. In more severe cases, the use of drugs with greater analgesic potential but which present a risk of dependence may be indicated;
– Arthroscopic debridement: performed through small incisions in which the doctor can visualize the inside of the joint and remove only the necessary tissue, relieving joint pressures;
– Osteotomy: a procedure in which a cut is made in the bone and repositioned with screws to realign it;
– Arthroplasty: surgery that replaces the injured joint with a prosthesis. The body regions that undergo arthroplasties are the knee and the hip;
– Arthrodesis: the procedure that performs a fusion between the joints through pins so that there is no movement between them. Usually, it is performed on the spine or foot;
– Custom insoles and shoes: custom-made insoles and shoes help realign the base of our body, improving the alignment of joints such as ankles, knees, and hips, affected by the body load.
There are cases where the pain is still intense, even with oral medications and physiotherapy. In these cases, medication injections directly into the joint, known as infiltrations, may be indicated mainly in the knee. Corticosteroids (a potent anti-inflammatory drug) or hyaluronic acid (a lubricating component of synovial fluid that increases cartilage nutrition) are usually employed. This is an invasive procedure; It should be prescribed and applied only by physicians.
Surgery will be indicated when joint wear is advanced, preventing joint movement that causes much pain. Some types of procedures can be performed for arthrosis management, such as arthroscopic debridement, osteotomy, arthroplasty, and arthrodesis.
FEET WITHOUT PAIN® CUSTOM SHOES AND INSOLES FOR ARTHROSIS
Feet Without Pain custom-made insoles and shoes promote the ideal alignment of the feet, ankles, knees, and eventual inequality of limbs. During the evaluation, our specialists check the limb length if necessary. In addition, technological equipment will be available to identify foot misalignment and the exact shape of the feet.
Thus, bone alignment will be corrected, leaving the joint surfaces with an evenly distributed load. Insoles and shoes will reduce overload and, consequently, inflammation in the joints, helping to improve pain and reducing the joint’s surface wear progression. In addition, they better promote plantar pressure distribution and impact cushioning. They are a powerful tool to reduce the symptoms that arthrosis causes.

The custom insoles and shoes are made with 3D technology and millimetric digital precision after a free foot, ankle, and knee evaluation with our specialists at one of our branch offices. Check some of their benefits for your feet below:
- Elimination or reduction of pain;
- Injury prevention;
- Increased comfort;
- Perfect fit;
- Standing longer without pain or discomfort;
- Prevention of pathologies progression;
- Improved impact absorption;
- Improved sports performance.

FOOTWEAR
On any occasion, footwear should always be chosen for comfort and not just for aesthetics. High-heeled shoes, for example, will concentrate the load exerted on the feet and misalign the joints, leaving them less able to cushion the load. Therefore, whenever possible, these types of shoes should be avoided.
This does not mean ballet flats or dress shoes should be banned, but we should always know when to use them. In cases where the feet will not be overloaded, the range of choice expands. But when the activity requires more time standing with possible overload, try to choose shoes with good cushioning.
More important than the shoe choice, paying attention to its wear in osteoarthritis is essential. A worn-out shoe that will throw your posture off balance can be more damaging than a cushioning-lacking shoe.
SPORT
Research proves the increased risk of arthrosis in elite athletes precisely because of the training overload. In addition, there is a higher prevalence in older athletes who practice sports with a higher trauma risk, such as American football, rugby, and ice rockery, as these are sports with greater physical contact and a chance of trauma. A higher rate of arthrosis was observed in the soccer players’ knees due to increased injury incidence to the menisci and ligaments.
The probability of injury and joint wear increases in high-impact sports. However, how the movement is executed, in this case, is more important than the load itself. Well-accompanied sports practice, with progressive training and movement correction, can reduce the chances of injury, thus decreasing the risk of arthrosis.
TIPS AND CURIOSITIES
– Appropriate equipment: protective equipment, especially in activities with more physical contact, is essential;
– Warming up and cooling down: preparing the body for any activity is essential. It increases muscles’ blood flow, making them more prepared for the action. Cooling down after physical activity helps the body to reorganize itself, and all systems need to return to resting level;
– A good teacher: the trainer corrects the movements, shows the proper sporting technique, and sets up a workout with ideal load progression, which is indispensable to prevent osteoarthritis;
– Decrease activities during pain: reduce activities during episodes of pain. When we feel pain, our body adopts postures to protect itself. This posture can lead to misalignment and worsen joint congruence. You will risk the misaligned joint if a high level of training is maintained;
– Stay active: practicing physical activity is essential to maintain good muscle strength and regulate metabolism, factors that can directly influence arthrosis. Some measures can be taken to maintain healthy physical activity;
– Ice compress: ice can be used for more intense pain. Because it is a more systemic disease, where more than one body system is involved, it is crucial to have a medical follow-up of the symptoms as soon as the disease is diagnosed. However, ice is an effective ally for quick pain relief. Apply the ice pack on the pain site for 15 to 20 minutes. Remember to protect the region with a thin cloth and never put ice directly on the skin.
Attention, it is possible to find teas to treat arthrosis on other websites. Some are rosemary, willow, and meadowsweet teas; Epsom salts and natural oils are also often cited. However, we must remember that these homemade tips do not have scientific evidence. The placebo effect is believed to be responsible for pain relief when using these resources. In case of pain, look for a specialist.
FREQUENTLY ASKED QUESTIONS (FAQs)

How to purchase your custom shoe or insole?
It’s fast and easy! Schedule a free evaluation of your feet with our specialists to buy your custom-made shoe.
Call, send a message to WhatsApp at 4003-8883, or visit: www.pessemdor.com.br/agendamento.
How does the evaluation work?
Upon arriving at a Feet Without Pain branch office, you will be received by a foot, ankle, and knee specialist, who will then fill out a registration form and ask some questions about your pain. Next, the assessment of the feet begins.
The specialist will examine your feet to understand your foot pains and complaints. Then, using the high-precision 3D scanner device, the specialist captures your feet’ measurements.
We are the only company with a 3D scanner for designing custom shoes. First, with the measurements of your feet, a mold is created using 3D printers, and after that, we start making your shoe.
How long does it take for the shoes and insoles to be ready?
Feet Without Pain produces custom-made shoes in up to 3 days; then, they are sent to your home free of charge!
Is the evaluation free?
Our assessment is completely free! We perform a complete analysis of your feet and legs, and you pay nothing for it!
Do we accept medical insurance?
We do not work with insurance because our assessment is completely free! But you can check if your plan somehow refunds you regarding the shoes!
EXTERNAL LINKS
1) Osteoartrite (Artrose): Tratamento | Scielo
2) Osteoarthritis of weigh bearing joints of lower limbs in former élite male athletes | NCBI




